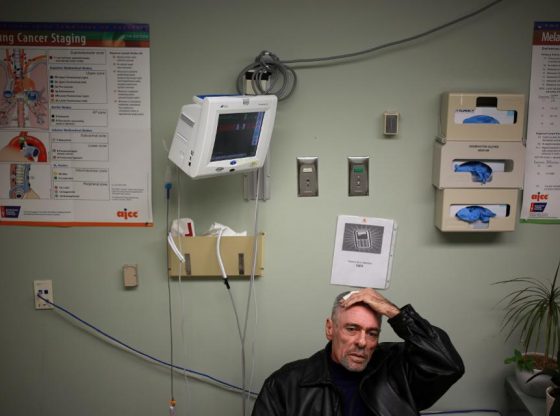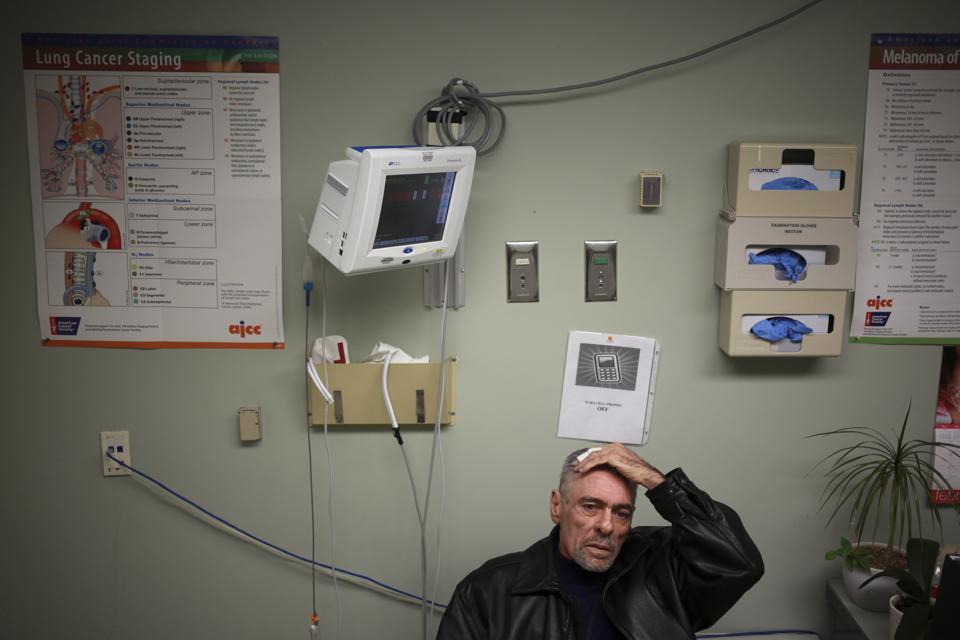
You have cancer. Your treatment is difficult, laborious, expensive, and stressful- even on even the best of days.
Enter, coronavirus. What now?
This is the difficult question that oncologists from all over the world are grappling with: how can we best care for cancer patients in an uncertain and dangerous healthcare environment, i.e. one that’s lurking with SARS-CoV-2, the virus that causes COVID19?
The answer is messy, unclear, and unsettling. While testing for SARS-CoV-2 in the United States is currently very limited, data from Wuhan show that patients with cancer are at higher risk of developing a serious case of COVID-19. This is cause for concern for both physicians and patients. “Overall, many cancer patients are scared and confused and, in some cases, angry,” says Stacey Tinianov, a 6-year breast cancer survivor and board-certified patient advocate living in Santa Clara, California. “The current guidelines regarding COVID19 testing, as well as cancer treatment continuation, pause and/or suspension, are still being ‘written’ and the statistics are remain very unclear.”
Ms. Tinianov is referring to the lack of clear cancer treatment guidelines for physicians to follow. The guidelines haven’t been written yet, because the pandemic is new and unprecedented. Who should continue, stop, delay, or initiate treatment isn’t always easy to identify. In the meantime, physicians who have some experience with COVID-19 have been sharing their invaluable experiences on Twitter, Facebook, WeChat and other social media platforms, so that healthcare workers elsewhere, who haven’t yet faced the pandemic surge, will be better prepared.
Dr Gil Morgan MD, a U.S.-trained oncologist practicing in Sweden, and Dr Felipe Ades MD PhD, an oncologist in Brazil, co-hosted a roundtable discussion on the social network #OncoAlert (of which I’m a member) on March 18th 2020. Oncologists from Italy, Sweden, Brazil and the U.S. shared information and best practices from the frontlines- i.e. information that without these social media tools, would take months to gather and share.
“The generosity of our Italian colleagues, in particular, and subsequently from other countries to generously share their experiences with us and warn us about very concerning health outcomes on a large scale and how best to prepare, has been a tremendous experience. The global medical community and even beyond coming together more closely represents already a remarkable positive effect arising from this harrowing crisis” said Dr. Nicole M. Kuderer MD MS, an oncologist in Seattle, Washington.
What information do cancer experts feel strongly about at this time? The reasons why both the elderly and cancer patients are at high risk for COVID-19 infections may be similar: older age, immunosuppression, and concurrent health problems.
Since the best way to slow down the virus is to limit social interaction, the fewer times a patient leaves their home, the better. For patients on active cancer treatment, Dr Gilberto de Lima Lopes Jr, MD, MBA, FAMS, a medical oncologist and Associate Director for Global Oncology at the Sylvester Comprehensive Cancer Center at the University of Miami, recommends screening patients when they enter the hospital for doctors visits and cancer treatment. “It’s extremely important that institutions start screening everyone who walks in for any respiratory symptoms and isolate and diagnose and test accordingly. I can’t emphasize enough the need for more testing,” Dr Lopes says.
The American Society of Clinical Oncology published FAQs for its members about how to minimize COVID19 risks for healthcare workers and patients. The American Society of Radiation Oncology published guidelines for radiation oncologists and patients receiving radiation. Recommendations from medical professional societies can be helpful to physicians, but it’s important to realize that individual hospitals have variable resources, including access to personal protective equipment for healthcare workers.
“I think it’s important to get the message out for patients to discuss with their care teams what makes the most sense,” Dr Lopes says. Oncologists must make difficult decisions when deciding how to advise their patients- each patient’s cancer is unique and many treatment are time-dependent. Patients must also weigh these trade-offs: should they stay at home and limit their exposure to coronavirus? Or, proceed with cancer treatment anyway?
Janet Freeman-Daily, a writer and lung cancer patient/activist shared “I know many patients with lung cancer whose cancer is progressing. They’re trying to decide whether to have a bronchoscopy, start chemotherapy, pursue clinical trials, or just wait a few months to see what happens. Tough choices when entering a hospital increases exposure risks.”
Additionally, many clinical trials for cancer patients have been disrupted during the pandemic, which is especially worrisome for patients who have run out of other cancer treatment options. “The biggest impact I’ve seen is in the metastatic community, where many people are on clinical trials and concerned not only with the challenges of those in-treatment but the very real possibility that their clinical trial, and the therapy keeping them alive in some cases, will be halted” says Stacey Tinianov.
The uncertainty facing cancer patients should, at minimum, remind the general public without cancer to take social distancing seriously. “We need to change our lives instantly and adopt- hopefully temporarily- a new way of living, using social distancing and self isolation at home,” said Dr Petros Grivas, MD PhD, an oncologist in Seattle, Washington. “Despite this being contradictory to our inherent social nature, it is urgent to follow the rules and guidance from scientists and experts. We need to pursue strict measures of self hygiene and avoid any crowding in order to “flatten the curve” and reduce the pace of virus transmission. The goal is to buy time, avoid overwhelming our health care systems worldwide, and save as many lives as possible.”
[“source=forbes”]