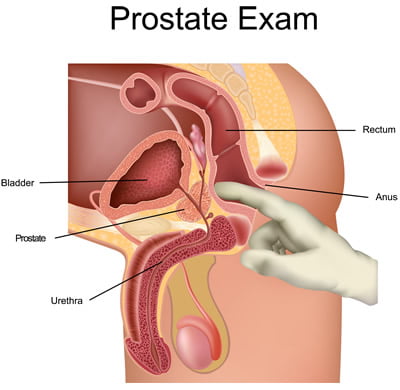
GPs should urgently refer patients with prostate cancer symptoms regardless of their digital rectal examination results, a new study has suggested.
Researchers from Hull York Medical School found that many men diagnosed with prostate cancer do not have an abnormal DRE result, so concluded that performing the examination in primary care is ‘unecessary’ and may even delay diagnosis by detering some men with symptoms from seeking medical help.
The systematic review, published in BMC Family Practice, found that patients with symptoms who have a normal result upon the physical check still have a 15.8% risk of cancer, well above the 3% risk threshold suggested by NICE for an urgent referral.
GP leaders called for more research to support the ‘interesting’ findings, before any changes to current recommendations for digital rectal examinations.
The research team set out to determine the accuracy of rectal examinations for prostate cancer diagnosis, in patients presenting to their GP with symptoms.
The review included four studies from 2015 which passed the quality assessment scale. A total of 3,225 patients were included, with the age of patients ranging from 40 to 89 years.
The research team, led by the dean of Hull York Medical School Professor Una Macleod, a former GP, looked at the sensitivity and specificity of the examination, as well as the cost-effectiveness and adverse effects.
They found that while DRE performed in general practice is accurate, ‘many patients diagnosed with prostate cancer do not have an abnormal DRE’.
The paper said: ‘Symptomatic patients who present to primary care and have a normal prostate examination still have a risk of cancer of 15.8%, which above the 3% risk threshold suggested by NICE…
‘DRE performed in primary care is an unnecessary investigation, adding little to the decision to refer, which should be made on the basis of symptoms alone.’
It added: ‘This review questions the benefit of performing a DRE in primary care in the first instance, suggesting that a patient’s risk of prostate cancer based on symptoms alone would warrant urgent referral even if the DRE feels normal.’
The researchers also suggested that ‘DRE may deter some men from seeking medical help for symptoms suggestive of prostate cancer…performing DRE in primary may in fact be delaying the diagnosis of prostate cancer’.
The University of Hertfordshire’s Professor Mike Kirby, a former GP with a special interest in men’s health, said: ‘A normal DRE of course does not exclude prostate cancer, but failing to do one misses the opportunity to diagnose locally advanced disease, and prioritise the referral, but also pick up other pathologies such as prostatitis, BPH, rectal tumours.’
RCGP chair Professor Helen Stokes-Lampard said: ‘This review certainly presents some interesting ideas…Improving rates of early diagnosis of prostate cancer is hugely important, but more research is needed before there is a change to the current recommendations about when to carry out a digital rectal examination.’
She added that it is ‘essential’ that for any updates to clinical guidelines, which are used by GPs to inform their diagnosis and treatment plans, that a ‘variety of the most current medical research and evidence’ is considered.
The findings come after Prime Minister Theresa May announced a £75m investment to support new research into early diagnosis and treatment of prostate cancer.
This will fund more than 60 studies in prostate cancer over the next five years to test treatments, such as more precise radiotherapy, high-intensity focused ultrasound and cryotherapy, coupled with exercise and dietary advice.