Divide and conquer – can metastasis be controlled? When a tumor migrates to another part of the body, it makes cancer much more difficult to…
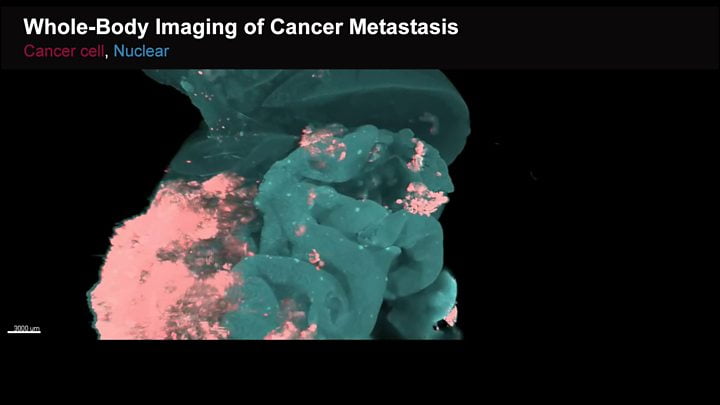
The way in which every single cancer cell spreads around the body has been captured in videos by a team in Japan. The normal body…
Scientists at the University of York have discovered that parasites responsible for leishmaniasis – a globally occurring neglected tropical disease spread by sand flies –…